MyMedicare practice implementation guide
- Introduction: the 5 steps to preparing your practice
- Step 1: Start with up-to-date patient information
- Step 2: Understanding your practice population and patient demand
- Step 3: Determining how many patients each GP could register
- Step 4: Understanding how many patients see each GP
- Step 5: Balancing supply vs demand in your practice
- Support contacts
Introduction: the 5 steps to preparing your practice
The following content has been adapted from the Brisbane South PHN Person Centred Care Toolkit: From principles to practice, 2019 developed by Australian General Practice Accreditation Limited (AGPAL). To view more and access the full content, please register for DiscoverPHN, our free online learning portal.
Understanding your practice’s current patient population and capacity to manage their needs is central to MyMedicare. There are 5 foundational steps for success in implementing MyMedicare for the benefit of your practice, your providers, and your patients.
1. Start with up-to-date patient information
Marking ‘inactive’ patients
This step ensures that you know who your active patients are and who might be eligible for MyMedicare registration with your practice.
Cleaning up clinical coding
This step allows for the identification of patients with specific conditions who might benefit from MyMedicare registration.
2. Understanding patient demand at your practice
This step helps you understand how many appointments your patients require.
3. Understanding how many patients each GP can register
This step helps you understand how many patients each GP can register based on their capacity.
4. Linking patients to a General Practitioner
This step allows you to monitor the number of patients assigned to each GP and identify those not assigned to a GP in your software.
5. Balancing clinician supply against patient demand in your practice
This final step looks at addressing any imbalances between patient demand and clinician supply to better balance GP workload and patient access to care.
Track your progress
Download our checklist to help keep track of your progress through the 5 steps.
Step 1: Start with up-to-date patient information
It is important to start with accurate information to help you understand which patients see your practice regularly and which patients might be eligible for MyMedicare registration with your practice. Additionally, keeping your practice data updated and accurate makes it easier to meet your ongoing accreditation and PIP QI requirements. Brisbane South PHN have a dedicated team of quality improvement coaches that can support your practice with quality improvement initiatives. Find out more at support@bsphn.org.au.
Notes:
*Total patients represent the number of unique patient identifiers (IDs) in your clinical software that have not been archived.
**Active population represents the portion of the total population that meet the RACGP Accreditation Standards for General Practice definition of an ‘active’ patient. This is patients who have had at least 3 visits to your practice in the last 2 years.
Activity 1: Marking ‘inactive’ patients
You can mark a patient ‘inactive’ within your clinical software if they do not meet the RACGP definition of an active patient or if they inform you that they will be moving away, are deceased or are only visiting due to travel or otherwise.
Please note: when archiving a patient, it does not delete them from the practice database.
Practice software instructions:
How to mark inactive patients using Best Practice
How to mark inactive patients in MedicalDirector
Activity 2: Cleaning up clinical coding
Ensure commonly diagnosed chronic conditions are coded using the pre-programmed drop-down lists within your clinical software. This will allow you to easily find information by searching specific conditions in your clinical information system or auditing tools. If you have used free-text instead of these pre-programmed lists, you may miss opportunities to provide items of care to patients who meet the eligibility criteria.
Practice software instructions:
How to clean up clinical coding using Best Practice
How to clean up clinical coding using MedicalDirector
If you need help with this step or your practice uses a different software product, please get in touch with us for support at support@bsphn.org.au.
Step 2: Understanding your practice population and patient demand
This step helps understand how many appointments are needed to meet the requirements of your patients. This can be called the patient ‘demand’ and helps to understand patient access to appointments in your practice. In later steps we will look at your patient demand versus how many patient appointments your GPs can provide (supply). Balancing supply and demand will help to improve patient access and help GPs manage their workload.
For further information on understanding supply vs demand in your practice, you can see the Patient Registration module from our Person Centred Toolkit: From Principles to Practice on DiscoverPHN.
Notes:
*Patient demand is defined as the known and anticipated needs of patients (i.e. how many appointments do your patients need).
**Supply is defined as availability of clinician appointments to meet patient demand.
Calculating patient demand requires an understanding of:
the number of active patients in your practice. You can easily identify the Number of Active Patients from within Primary Sense.
the total number of patient visits to all GPs within your practice in the last 12 months.
Report the total number of visits in Best Practice
Report the total number of visits in MedicalDirector
the average number of appointments per patient per year. This can be calculated by dividing the total number of GP appointments per year by the number of active patients.
You can download this template, to record steps 2-5, to populate as you work through this process. Alternatively, individual templates are available under each step.

Step 3: Determining how many patients each GP could register
The aim of this step is to understand the ‘ideal’ number of patients that could be registered to each GP in your practice. This will help with understanding GP workload. This step looks at the supply of GP appointments available to your patients based on the number of days each GP works.
Calculating provider supply requires an understanding of:
The average number of appointments per patient per year.
Calculated above in step 2.
The total number of General Practitioners you have working in your practice.
Include all GPs who are seeing patients for general consults.
The number of general consult appointments each GP has available per year. Repeat this calculation for each GP working in your practice. There are different ways to calculate this; by day, week or month to get the annual total. Choose one of the methods below.
Calculating by day:
How many patient appointments does each GP have available per day they work? Do not include provision of specialty services such as skin clinics.
How many days do they work in your practice? Do not include administration time, education, leave or provision of specialty services such as skin clinics.
Multiply these 2 numbers to get the total number of appointments each GP has available per year.
Calculating by week:
How many patient appointments does each GP have available per week they work? Do not include provision of specialty services such as skin clinics.
How many weeks do they work in your practice? Do not include administration time, education, leave or provision of specialty services such as skin clinics.
Multiply these 2 numbers to get the total number of appointments each GP has available per year.
Calculating by month:
How many patient appointments does each GP have available per month they work? Do not include provision of specialty services such as skin clinics.
How many months do they work in your practice? Do not include administration time, education, leave or provision of specialty services such as skin clinics.
Multiply these numbers to get the total number of appointments each GP has available per year.
The Best Practice Appointment Statistics Report shows GP appointment information by month.
The MedicalDirector Monthly Visit Summary by Practitioner Report shows the number of patient visits recorded per month for each GP.
Use our calculator tool to assist in working this out. You will need to do this calculation for each GP who works in your practice.
You can record this on this Step 3 template
Working example:

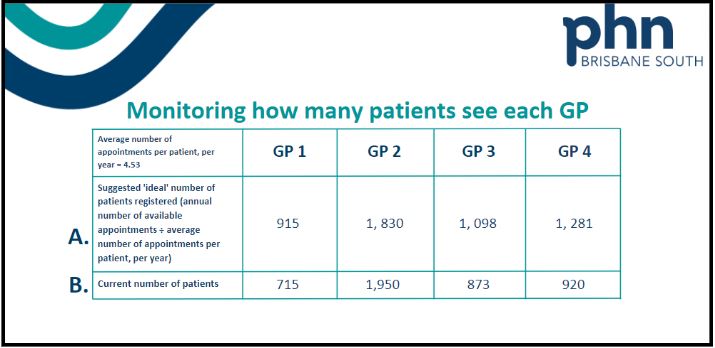
Step 4: Understanding how many patients see each GP
The aim of this step is to ensure your patients’ registered GP is recorded in your clinical software to help understand how many patients each GP is currently seeing. This will help with billing items related to MyMedicare.
MyMedicare formalises the relationship between a patient and their preferred GP. Some patients may have seen multiple GPs at your practice. This is still permitted under MyMedicare, though in future certain care items such as GPMP will be tied to patient’s MyMedicare registered provider. The patient choice must be upheld in deciding who is their registered MyMedicare GP.
Now that we have calculated an ‘ideal’ number of patients that could be registered to each GP (Step 3 above) it can be useful to report on the actual number of patients currently seeing each GP.
Calculating how many patients currently see each GP:
You can use your clinical software to understand how many patients are regularly seeing each of your GPs.
Identifying current patient population for individual GPs in Best Practice. (Select the Patient – Current List report and use the parameters to select the GP).
Identifying current patient population for individual GPs in MedicalDirector.
You can record this on this template.
Using your clinical software to record the patient’s preferred GP
To assist with easily identifying a person’s registered GP for booking and billing appointments, you can use the provided fields in your clinical software to record a patient’s preferred GP.
Set a usual provider in Best Practice (scroll down to ‘Set a usual provider’). See our guide here.
Set a regular practitioner in MedicalDirector
Tips:
Best Practice Premier Orchid software has a specific MyMedicare registration status checkbox also to help capture patients who are registered for MyMedicare.
If your practice has Cubiko software, there is now a MyMedicare function that supports practices to perform bulk updates of MyMedicare registration status integrated with Best Practice.
Quality Improvement activity to capture preferred GP
If your practice has not routinely been entering a patient’s preferred GP, our Quality Improvement coordinators can help you complete an activity as a team to ensure your active patients have their preferred doctor recorded. Please phone our QI team on (07) 3864 7540, or email support@bsphn.org.au
You can start by identifying patients that do not have their preferred doctor recorded.
Best Practice Supplied Database Query Patients without a usual doctor set
Medical Director New Patient List by Practitioner.
This report will list all patients that have a regular practitioner listed. You can compare this to a Full Patient List Report to determine patients who do not have a regular practitioner specified.
Step 5: Balancing supply vs demand in your practice
The aim of this step is to achieve a fair and equitable balance of expected patient demand across all GPs in your practice. Once you have determined the current number of patients a GP sees (calculated in Step 4), it is then useful to compare this against the ‘ideal’ number of patients each GP could register (calculated in Step 3 above). Calculating the difference between the current number of patients registered to a GP and the ‘ideal’ number of patients registered to a GP helps to understand supply and demand better. You may see a need to distribute patient demand better across your providers. This is important to help meet patient needs and manage GP workload.
Tips:
You can record them on this Step 4 & 5 template.
Working example:
 A positive number may indicate that the GP could see that many more patients, while a negative number indicates that GP is seeing more patients than they can meet demand for.
A positive number may indicate that the GP could see that many more patients, while a negative number indicates that GP is seeing more patients than they can meet demand for.
NOTE: These numbers are indicative only. Conversations with GPs are needed to clarify their patient demand and workload.
These activities may have yielded some interesting insights into your GP capacity and workload. If you have some GPs that have more patients registered to them than they can reasonably care for, it might be worth having conversations with patients and GPs about reassigning some patients to another GP who might have better capacity to manage their health care needs.
You can read more about this in our Patient Registration module on DiscoverPHN. This is module 6 in our Person-Centred Care Toolkit: From principles to practice.
Support contacts
Contact Brisbane South PHN for support via support@bsphn.org.au or phone 1300 467 265.
Our Quality Improvement Team can be contacted directly by phoning (07) 3864 7540.