Palliative care
- Brisbane South PHN 3 Year Palliative Care Action Plan 2023-2025
- Prompts for End-of-Life Planning (PELP) Framework
- End-of-life care in residential aged care facilities
- Metro South Palliative Care Service
- Paediatric Palliative Care Service
- Palliative care referrals
- Palliative Care Queensland
- PallConsult
- ELDAC Website and Resource Hub
- Support for families and carers
- Advance care planning
- Quality improvement
- More information
Brisbane South PHN 3 Year Palliative Care Action Plan 2023-2025
Brisbane South PHN’s vision for people affected by life limiting illnesses in communities across Brisbane South is for people to get the care they need to live well.
Our priority areas for action to achieve this:
increasing death literacy and understanding of dying well in priority communities across Brisbane South
improving the accessibility and equity of palliative care services and supports
strengthening the delivery of palliative care to be holistic, effective, high-quality and responsive to people's needs
supporting a capable palliative care workforce, particularly primary health and aged care services
building an integrated, informed palliative care system
To deliver on our Action Plan, Brisbane South PHN will:
establish governance mechanisms that provide clinical oversight, involve consumers and carers, and guide the implementation and review of the plan
work in partnership with key stakeholders across the region, such as Metro South Health, general practices and primary care providers, aged care services, Aboriginal and Torres Strait Islander community-controlled services and community groups
provide targeted resourcing through our commissioning approach
undertake monitoring and evaluation of the Action Plan to collect data, measure outcomes and identify learnings
develop reporting that shares insights with key stakeholders in our region and contributes to building the evidence base.
Prompts for End-of-Life Planning (PELP) Framework
The Palliative and End-Of-Life Care Framework – Last 12 Months Of Life guides proactive, quality end-of-life care across all care settings.
The PELP Framework contains prompts that support:
Identification of patients suitable for a palliative approach to care:
Ask the surprise question: ‘Would you be surprised if the person died in the next twelve months? This can be answered by intuition , using clinical and personal knowledge of the patient, and/or clinical tools (e.g. SPICT).
Identification of four clinical end-of-life processes:
Advance care planning and person-centred care based on need (at risk of dying)
Transition focus of care needs from restorative to palliative (likely to die soon)
Terminal care needs (dying)
After-death care (bereavement).
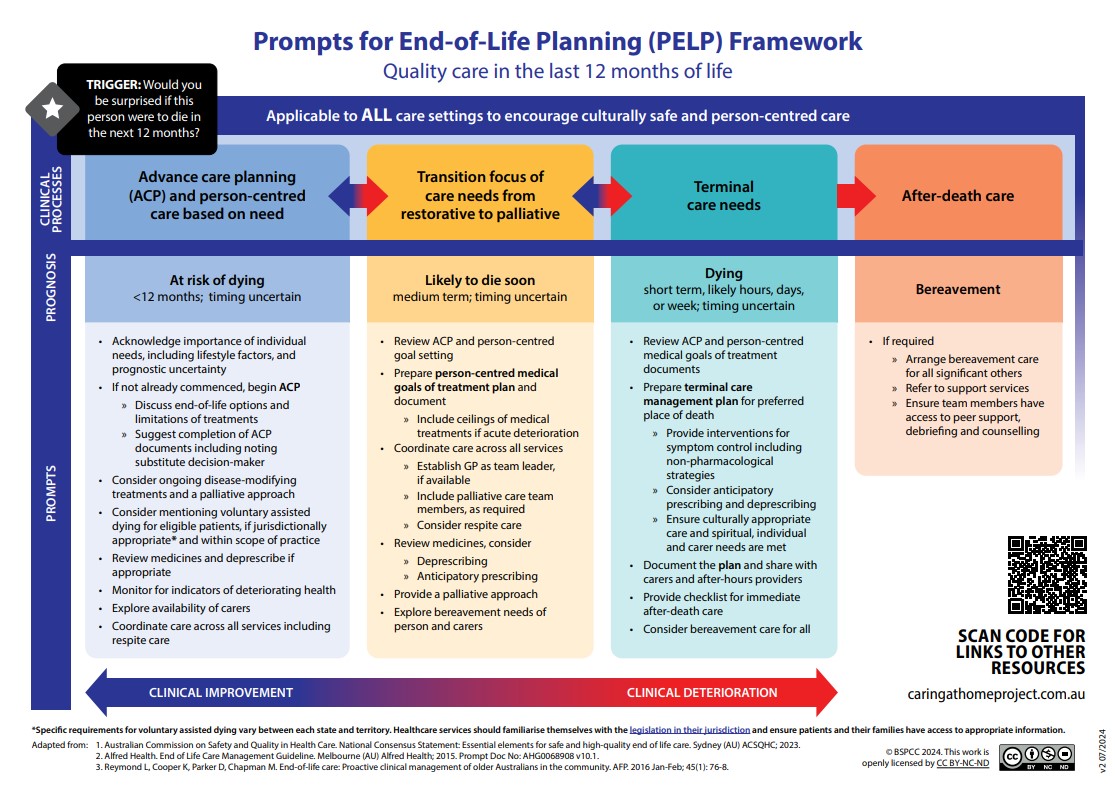
When to use it
Implementation of the PELP Framework helps health professionals deliver quality person-centred care in the last 12 months of life.
It encourages identifying patients at risk of deteriorating and dying, prompting meaningful conversations about their care goals and preferences. These ongoing discussions help create person centred management plans that reflect the person's wishes and reduce making difficult decisions during emotional times.
End-of-life care in residential aged care facilities
In 2017, the Improving End-of-Life Care Residential Aged Care Residents Initiative was developed by Brisbane South PHN in partnership with the Metro South Palliative Care Service (MSPCS). The initiative aims to support Residential Aged Care Facilities (RACFs) to embed evidence-based practice in their routine clinical care to support high-quality end-of-life care for residents and their families.
palliAGED https://www.palliaged.com.au/ is a national online resource offering evidence-based guidance, practical tools, and training to support palliative care in aged care settings. It assists health professionals, careworkers, and families in delivering quality end-of-life care aligned with Australian standards.
The recent Productivity Commission’s Report, ‘End-of-life care in Australia’, agrees that end-of-life care should be core business for RACF’s. However, it acknowledges this will require a coordinated approach in supporting the upskilling and ongoing education of aged care nurses to ensure they have the necessary skills to lead and coordinate end-of-life care in RACFs.
Palliative care is a responsive and holistic approach to care provided for a person with an active, progressive, advanced disease who has little or no prospect of cure and who is expected to pass away. The primary goal of palliative care is to optimise the person’s quality of life.
Metro South Palliative Care Service
In our region, the Metro South Palliative Care Service (MSPCS) provides specialist palliative care services including within the community, residential aged care facilities, public and private hospitals including working closely with the St Vincent’s Private Hospital Community Specialist Palliative Care Team.
The MSPCS works with Brisbane South PHN through the BrisbaneSouthHealthPathways initiative to facilitate integrated, local health care pathways for patients requiring palliative and end-of-life care.
Paediatric Palliative Care Service
The Children’s Health Queensland Paediatric Palliative Care Service provides physical, emotional, spiritual and psychological support to children who have a life-limiting illness. Care focuses on quality of life – it does not mean withdrawing all treatment. Active interventions such as surgery, chemotherapy and radiotherapy, medication regimes or special diets may help to relieve symptoms and improve a child’s quality of life.
The service also provides support to families (including siblings) of children with a life-limiting illness and arranges for palliative care to be delivered in various places, including the home, children’s hospital, local hospital or hospice.
Palliative care referrals
Refer to the following services:
Palliative Care Queensland
Palliative Care Queensland (PCQ) is an independent not-for-profit peak body representing palliative care providers, patients and their families, and those with an interest in palliative care in Queensland. They provide information about accessing Palliative Care services and support health professionals to provide quality palliative care.
PallConsult
The PallConsult is a Queensland Health service website and phone service providing 24/7 support to health care professionals without easy access to a palliative care service. PallConsult allows clinicians to speak with a specialist palliative care nurse at any time, day or night, and provide quality care for people approaching end-of-life and wishing to remain at home.
Call PallConsult
Phone: 1300 725 527
Hours: 24 hours a day, 7 days a week
ELDAC Website and Resource Hub
The End of Life Directions for Aged Care (ELDAC) Helpline is a free Australian Government service. ELDAC provides information, guidance and resources to health professionals and aged care workers to support palliative care and advance care planning to improve health care for older people.
Support for families and carers
The ‘Carer Gateway’ website is the Australian Government’s online portal to provide practical advice and access to supports for family members and friends caring for people with health conditions that demand a lot of support from their carer, including those with life-limiting illnesses. Services including support to connect with health services, free phone counselling, carer coaching and connection to other carers.
The CareSearch Community hub https://www.caresearch.com.au/Community provides trustworthy, easy-to-understand information about palliative care for patients, carers, and families. It offers practical guidance on living with illness, caring for someone, managing symptoms, and preparing for end of life, with resources tailored to diverse cultural needs and different stages of the journey.
Advance care planning
The ‘My Care, My Choices’ website is the Queensland Government’s online portal promoting the important processes of advance care planning and providing information and resources to the health professionals and the community.
Advance care planning involves informing and educating your patients about their ongoing health care options specific to their needs, then supporting their decision making. Advance care planning may be general or require specific advice about an Advanced Health Directive, Enduring Power of Attorney, Statement of Choices or forms to revoke these documents.
Quality improvement
Brisbane South PHN has a quality improvement toolkit designed to support health professionals to provide quality palliative and end-of-life care.
More information
Visit our Practice Support pages.




