Improving pneumococcal and influenza vaccination rates for patients with COPD
For the one in three Australians living with a lung disease, vaccine preventable respiratory infections increase their risk of symptom exacerbation, lung function deterioration, hospitalisation and death.
In Australia, adult vaccination coverage for the vaccine-preventable respiratory diseases (influenza, COVID-19, pneumococcal pneumonia and pertussis) is sub-optimal.
This activity will focus on improving the recording and uptake of pneumococcal and influenza vaccinations in patients with COPD.
Through trying small changes and ensuring we have a process for providing evidence-based vaccination schedules for patients with COPD, we’re reducing the risk of harm from preventable respiratory illnesses for our high-risk patients.
QI activity overview
Overview
What is the aim of this QI activity?
Improve vaccination coverage for vaccine-preventable respiratory illnesses for our patients with COPD.
Identify and recall 10 patients with COPD that are due an influenza and/or a pneumococcal vaccination.
What will I need to do?
Use Primary Sense reports to identify 10 patients with COPD that are due for an influenza and/or a pneumococcal vaccination.
Review immunisation history on Australian Immunisation Register (AIR)
Contact the patient to arrange an appointment.
Document immunisation information.
How will I complete this activity?
Identify who in the practice will search for eligible patients, check immunisation history, administer the immunisation, who will document and track the results. Use the step-by-step guide below to assist.
Where do I document my results?
Who can I contact for support?
For support with this activity, please contact the General Practice Quality Improvement team on Ph. 38647540 or email: support@bsphn.org.au
Step 1: Start your activity
1. Identify patients with COPD
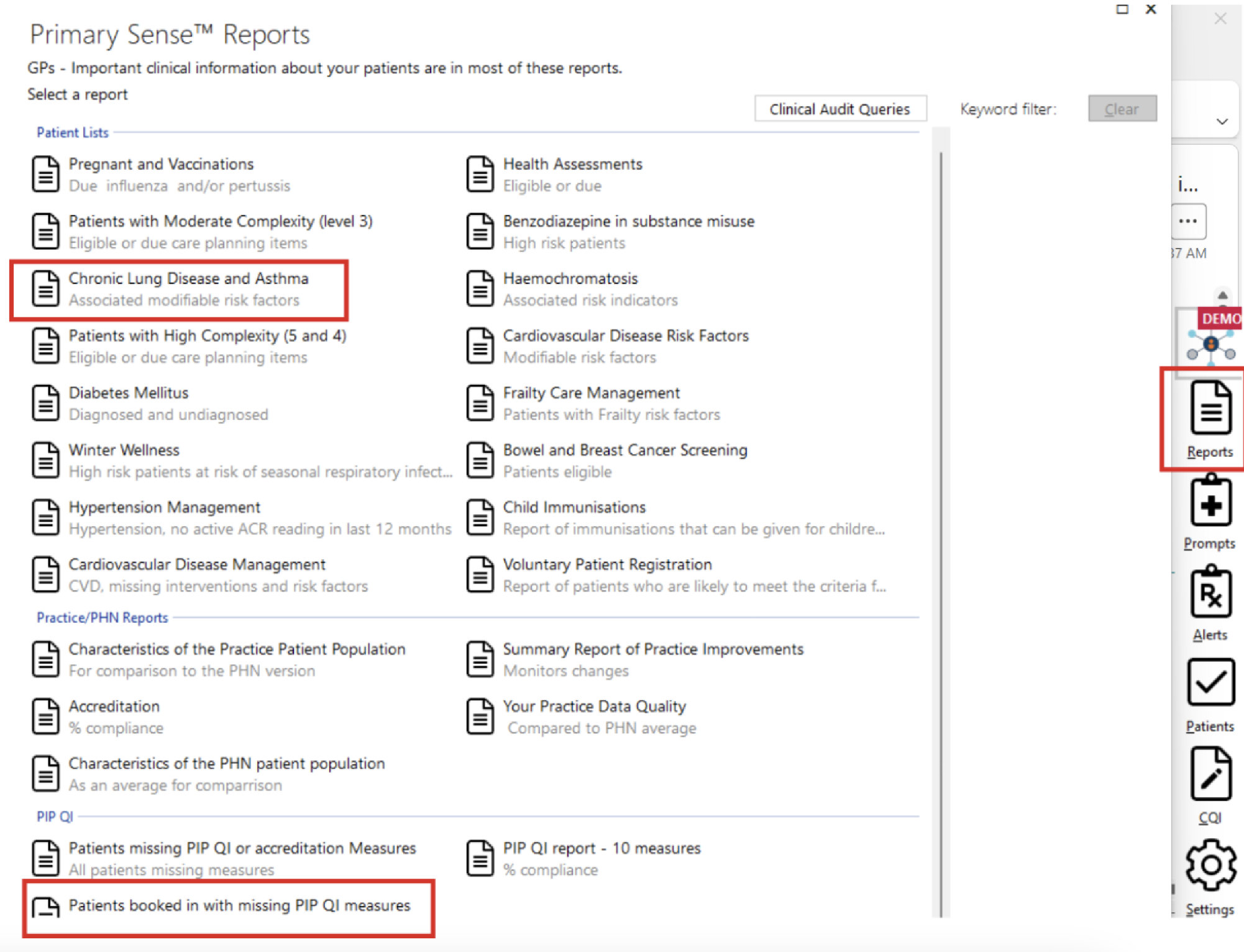
Using Primary Sense, identify 10 patients with COPD that have clinical records indicating they are due for an influenza and/or pneumococcal vaccination. To do this, we suggest using the Chronic Lung Disease and Asthma report and reviewing patients booked in with missing PIP QI measures.
Chronic Lung Disease and Asthma report
Using the search function, search for COPD or Chronic Obstructive Pulmonary Disease (depending on how your practice codes the condition). This will filter the report to those patients with a COPD diagnosis coded in their patient record.
The columns titled “History of Pneumococcal Vaccination” and “History of Fluvax” can then be used to identify patients that have do not have a current influenza vaccination and/or pneumococcal vaccination recorded in their clinical record. The arrows beside the columns can be used to filter by date.
Patients booked in with missing PIP QI measures
Column titled “FluVax due reason(s)” can be used to identify patients with COPD, diabetes and/or over 65 years that have an appointment in the next 2 weeks and do not have a current influenza vaccination (<15 months) recorded in their patient record.
To filter the report to patients with COPD, use the search function to search for COPD or Chronic Obstructive Pulmonary Disease (depending on how your practice codes the condition).
Tip: the Primary Sense report can be extracted for ease of use and saved as an excel file.
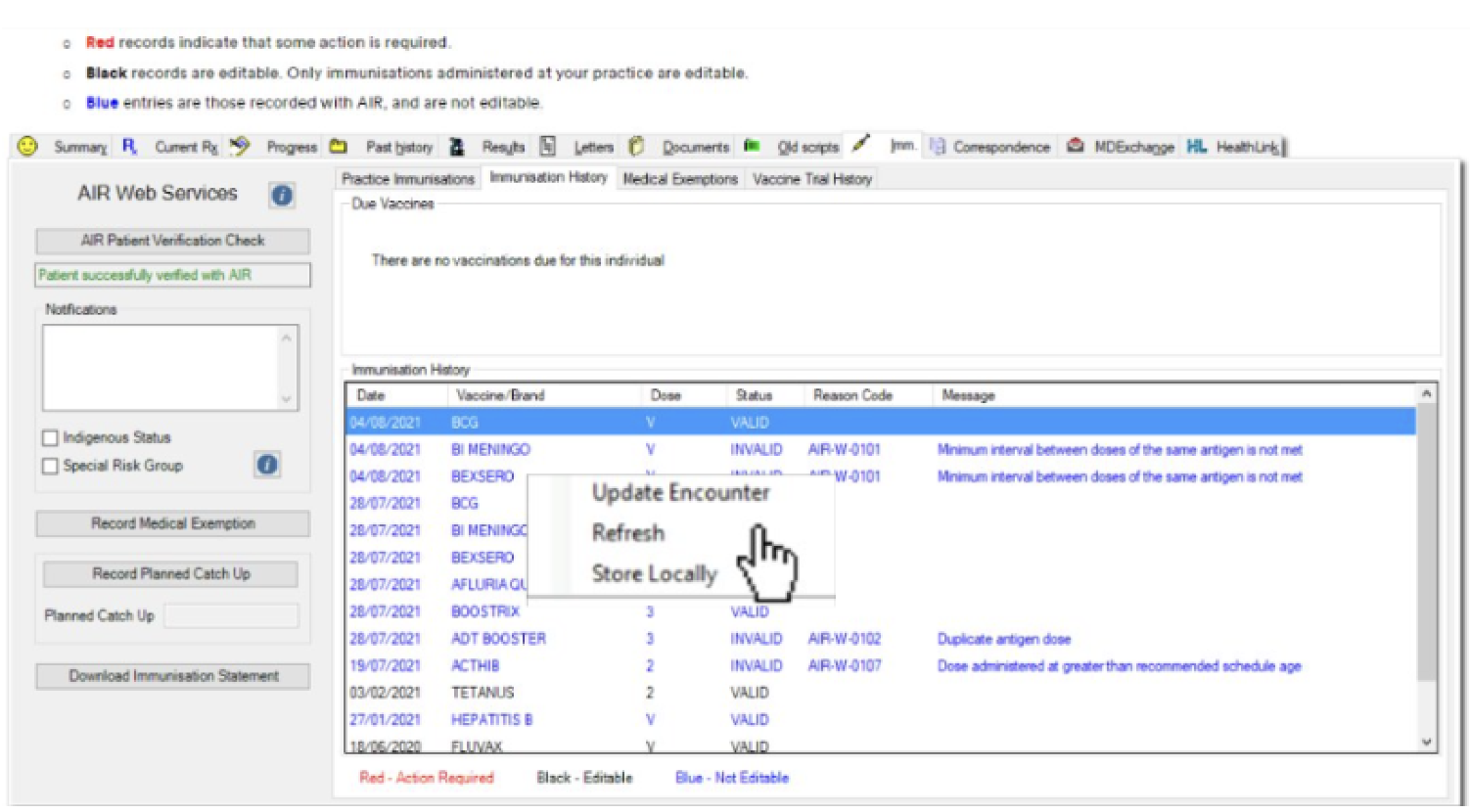
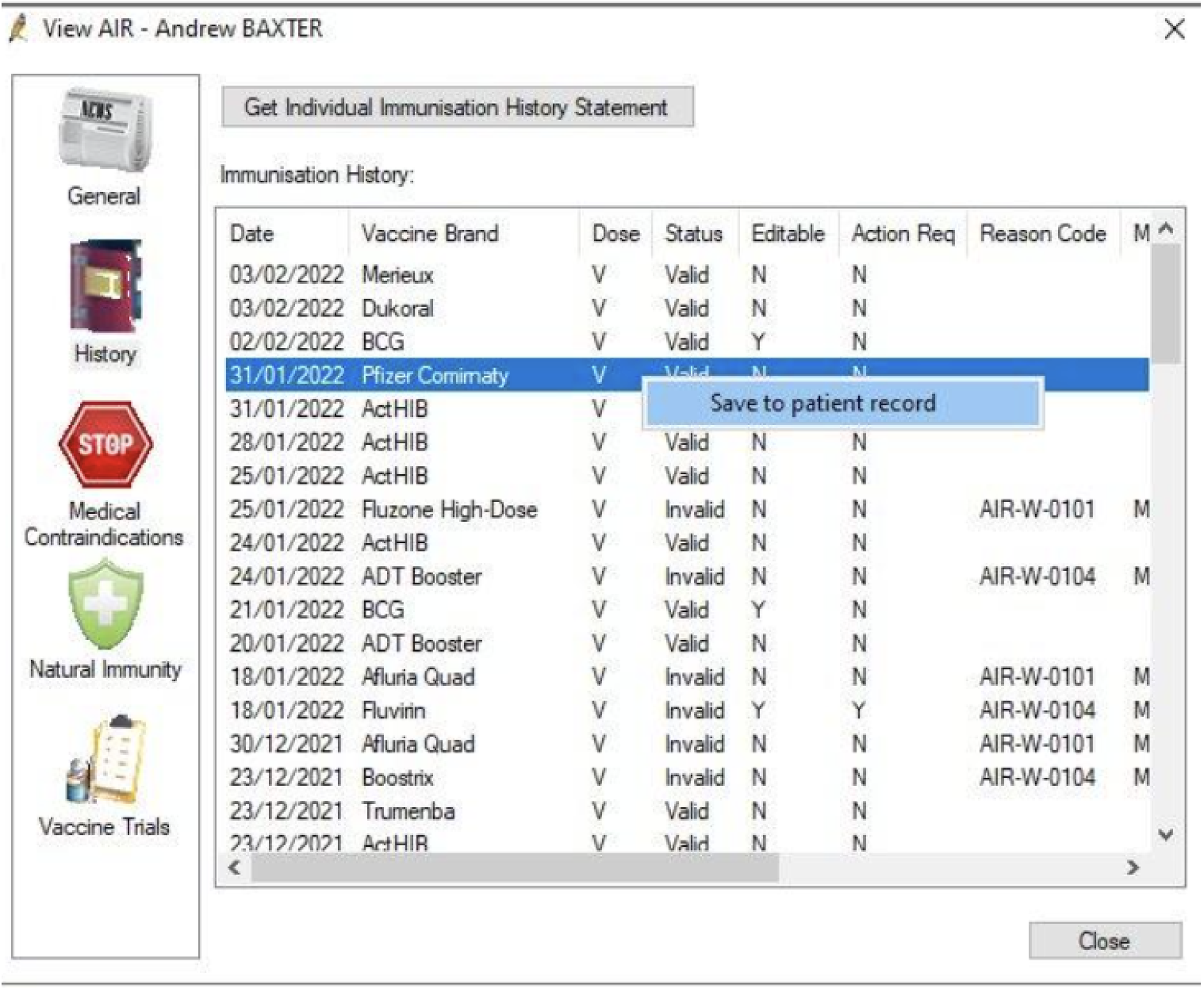
2. Review patient immunisation history
For the 10 patients identified in step 1, use your clinical software to access the Australian Immunisation Register (AIR) and view their AIR immunisation history. If applicable, save any missing vaccination record entries from AIR into the patient’s clinical record at your practice.
For MedicalDirector, right click on the vaccination record you wish to save and select “Store Locally”
For Best Practice, right click on the vaccination record you wish to save and select “Save to patient record”.
3. Contact your patients
Once immunisation history from AIR has been reviewed and patient records updated. Recall and/or set-up a reminder for 10 of your patients with COPD that are due an influenza and/or pneumococcal vaccination.
Potential ideas for recalling patients:
Phone the patient
Send an SMS reminder to the patient
Create an internal prompt in the practice clinical software for patients with appointments coming up in the next two weeks (the Primary Sense report can assist with this).
4. Document patient vaccinations
Prior to administering any vaccines provide patient with the Table. Pre-vaccination screening checklist | The Australian Immunisation Handbook.
After the vaccination has been administered, ensure this is documented in the immunisation section of the patient's file.
Record an immunisation in Best Practice - refer to instructions Record immunisations
Record an immunisation in MedicalDirector - refer to instructions MD Help.
Update recall/reminder system if future vaccinations are required.
5. Document Results
Document results of the activity. You can use the tracking posters to record results and display them in the treatment room or lunch room so that team members can see the impact of their changes. You can also document your results in the QI summary register or MFI/PDSA.
Step 2: Track your results
Tracking results
This section will assist you to track your results and answer the following questions:
How will you know that change is an improvement?
What data will be used to track the improvement?
What is the current data showing?
Suggested measures and data sources
Use the Primary Sense desktop report “PIP QI report – 10 measures’’ to record “QIM 6 – Patients with COPD who have been immunised against influenza”. The numerator for QIM 6 can be used pre and post activity for a comparison of the number of patients with COPD and a current influenza vaccination (<15 months) before the activity and after the activity.

Manually record the number of patients identified, recalled and provided an influenza and/or pneumococcal vaccination from the QI activity.
Step 3: Complete and reflect on your activity
How did you go?
As a team, reflect on how the activity went.
What were the challenges/barriers?
What worked well?
Are there any small changes that you could implement to continue improving vaccination coverage for your patients with COPD?
Share your results
Share your results with your team and Brisbane South PHN.
Need support?
Consider if there are additional patients with COPD you can contact to update their vaccination or consider another activity.
Example of completed QI activity
QI activity example
View the Model For Improvement (MFI) diagram and Plan, Do, Study, Act (PDSA) example of a practise aiming to increase their number of active patients with COPD who have an influenza vaccine.
Resources to support with your QI activity
Please find attached all of the tools and resources to support with your activity below.
Tools and resources
Model for Improvement/PDSA Template
QI Summary Register
Influenza target poster
Pneumococcal target poster
Roles and Responsibility: Team activity Worksheet
Best Practice instructions to link to Australian Immunisation Register
Chronic Conditions Manual: Prevention and Management of Chronic Conditions in Australia (Pg. 255)
Chronic Obstructive Pulmonary Disease - Clinical Care Standard 2024
Lung Foundation Australia - Respiratory Infections - For Health Professionals
Australian Immunisation Handbook
National Immunisation Program Schedule
Australia Immunisation Handbook - Pneumococcal vaccination for people with risk conditions for pneumococcal disease
We appreciate your feedback!
Our Quality Improvement Team works with general practices to provide practical advice and resources to help plan, implement, and review your QI activities. Your feedback helps our team to provide the best possible support for your practice.
Contact General Practice Quality Improvement
Phone: 07 3864 7540





